The Increasing Prevalence of Diabetes
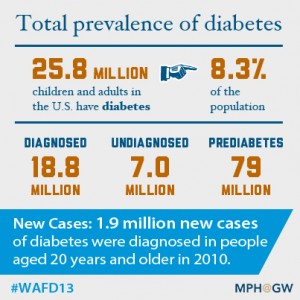
Diabetes is on the rise in the United States among both children and adults. More than 8 percent of the entire population has diabetes, approximately 25.8 million Americans, according to the American Diabetes Association. In 1958, there were only 1.5 million people diagnosed with diabetes as compared to 18.8 million in 2010. 7 million people are undiagnosed and 79 million have prediabetes.
Among youth, there has been a substantial increase in the diagnoses of both type 1 and type 2 diabetes — and 215,000 Americans younger than age 20 have diabete. According to a 2012 article published in the Chicago Tribune, the percentage of teens with early onset adult diabetes has “more than doubled in recent years.”
As a chronic condition in which the pancreas is unable to make enough insulin, diabetes may not appear to be a systemic disease. It is often managed by adhering to a strict diet low in sugar and/or insulin injection. However, there are numerous potential complications related to being diabetic, and the cost to the United States health care system is staggering. The high economic and clinical burden on the health care system has vaulted the prevalence of diabetes to a national public health issue.
Potential Health Complications
Over time, diabetes can have wide-ranging systemic consequences. The most frequent complication of longstanding diabetes is peripheral neuropathy — a tingling sensation or pain in the hands or feet. Retinopathy, which can lead to blindness, is another frequent complication. Additionally, a long duration of poor circulation to the feet typically leads to non-healing infections that can become gangrenous and result in amputations.
Diabetes is also a major cause of kidney failure that can lead to the need for dialysis, and subsequently, to a kidney transplant. However, the damage caused by diabetes to the original kidneys frequently occurs in the transplanted kidney. Therefore, patients whose initial kidney failure was due to diabetes have the worst long-term transplant outcomes of all recipients.
Other complications include a predisposition toward osteoporosis and atherosclerosis. The lack of well-controlled glucose levels exacerbates the development of disabling diabetic complications.
Economic Implications of Diabetes
The high national cost of diabetes is not only related to the medical management of the disease itself, but to its complications and effects on workplace productivity. Diabetic complications can lead to an inability to continue functioning in a work role — and disability claims are straining the Social Security system. In addition, seniors with longstanding diabetes often need nursing home care due to an inability to function at home without intensive support. The financial implications of nursing home care are acute for the families of residents.
The financial expenditures related to the overall diabetic management are staggering. In 2012, the total costs in the United States of diagnosed diabetes were estimated at $245 billion — a 41 percent increase over the past five years, according to the American Diabetes Association.
Prevention Efforts
Obesity is a major cause of type 2 diabetes, and weight loss at an early stage can reduce the need for pharmaceutical treatment. Public health efforts in the United States aimed at preventing diabetes have been closely related to preventing obesity and encouraging increased physical activity.
Small doses of exercise after meals may also help reduce the risk of developing type 2 diabetes, especially among the elderly. In a study published in Diabetes Care, Professor and Chair of Exercise Science Department Loretta DiPietro, Ph.D., found that a 15-minute walk after meals can help older people regulate blood sugar levels and decrease their risk of developing diabetes. Raised blood sugar levels can last for hours after a meal, but a short post-meal walk was found to be immediately effective in counteracting this damaging effect. Preventative strategies like this could make a big difference for the estimated 79 million Americans who have pre-diabetes.
While other studies have shown that exercise and weight loss can prevent type 2 diabetes, this is the first study to assess the effects of short bouts of moderate exercise on blood sugar levels after meals. The results of this study must be confirmed with larger trials, but this simple, inexpensive strategy may be one of the keys to diabetes prevention.
Disparities in Diabetes Incidence
People with low incomes are more likely to supplement their diets with high-caloric fast food and carbohydrates (such as potatoes) that decrease the sensation of hunger and are inexpensive. This diet makes low-income populations especially vulnerable to obesity and adult-onset diabetes.
The burden of diabetes in the United States is also much higher for minorities than for the white population, according to a fact-sheet of the Agency for Healthcare Research and Quality. Native Americans have the highest prevalence of diabetes in the U.S. of all racial groups at 16.1 percent, according to the American Diabetes Association.
The growing public health problems of obesity and diabetes in the United States are interrelated, and public health promotion efforts aimed at reducing the onset of diabetes in those most at risk are crucial to reducing its societal costs. Besides prevention efforts, early diagnosis and appropriate medical care can forestall some of the typical complications. Public health educators play an important role in addressing this debilitating and costly disease.

Join MPH@GW in our campaign to Walk Away from Diabetes! If you are a blogger who has a personal story or if you are someone advocating for diabetes prevention, consider sharing your perspective to raise awareness and let others know they are not alone in their struggle against diabetes.


